I’m okay with it. It’s just so normal to me now. It’s just brainwork, it’s so easy – I got to go, I go, and I’m out in, like, two minutes! It’s become very normal to me.
Kayla, age 14
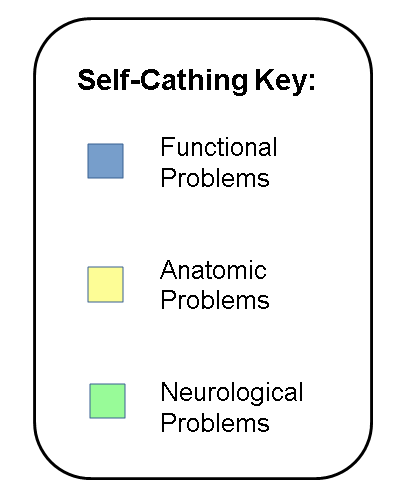
The Self-Cathing Experience Journal is a collection of stories and personal experiences from patients and families about what it has been like to use clean intermittent catheterization (CIC). CIC, sometimes called self-cathing, involves periodically emptying the bladder using a thin tube called a catheter when patients are unable to empty their bladders completely on their own. There are many reasons that patients may need to self-cath, falling into three basic categories:
- Functional problems involve bladder dysfunction without an anatomic abnormality or neurological disorder. Symptoms may be caused by recurrent infections, a history of holding urine, or other negative emptying patterns that disrupt normal bladder function. Functional problems are often temporary.
- Anatomic problems involve bladder dysfunction caused by atypical anatomy (e.g., bladder exstrophy, posterior urethral valves). Abnormalities are usually present at birth and may require corrective surgery. Children with anatomical problems affecting bladder function often need lifelong catheterization.
- Neurological problems involve damage to the nerves connecting the bladder to the brain, a condition known as neurogenic bladder. Common diagnoses include spina bifida and tethered spinal cord. Neurological disorders are usually present at birth, and may require corrective surgery and lifelong catheterization.
We have chosen to group these problems together and focus on the common experience of self-cathing. However, we have color-coded the self-cathing stories so that you may also read stories about a particular diagnostic category.
While it is normal to feel some emotional discomfort associated with reading the stories of children and parents describing their experiences with self-cathing, we hope that families may learn from the stories of others facing similar experiences.
Visit the Glossary to read definitions for words in bold. Visit our Resources page to learn more about family and clinician recommended websites on coping with self-cathing.
Video Interviews:
The following videos feature several adolescents and families talking about their experiences with self-cathing:
- Interview with Alexa, an adolescent
- Interview with Alexa’s mother
- Interview with Henry, an adolescent
- Interview with Henry’s mother
- Interview with Elizabeth, an adolescent
- Interview with Elizabeth and Dr. Lauren Mednick, PhD, a medical coping psychologist at Boston Children’s Hospital
The following videos feature clinicians from the Boston Children’s Hospital Department of Urology as they discuss their experiences working with patients and families who need to use CIC:
- Meet the some members of the Department of Urology Team
- Urology Programs at Boston Children’s Hospital
- What is CIC and why would someone need it?
- How do you talk to families about CIC?
- How do you help families accept CIC?
- How do you tailor treatment for individual patients?
- What are potential problems with using CIC?
- What are functional problems that may require CIC?
- What are neurological problems that may require CIC?
- What are the challenges and rewards of working with CIC patients?
Child & Adolescent Stories:
I just think you can’t let yourself be embarrassed, because it’s not your fault. And I let that hold me back from doing certain things when I was in elementary and the beginning of middle school, and I found that once I was honest with my friends, they didn’t care.
Elizabeth, 16
- First signs
- Trying other treatments
- Infections and accidents
- Self-Cathing: accepting, learning, and doing it
- Needing another way: Mitrofanoff Procedure
- How it affects my family
- How it affects my social life
- How it affects me at school
- Growing up with health problems
- My future health care
- Coping with stress
- Tricks of the trade
- Words of wisdom
Read Isaiah’s Story: Dialysis & Transplant
Caregiver Stories:
You can’t think too much about it or go on anyone else’s advice. You have to go on what you feel is right for your child, your family, and yourself as the caregiver.
Mother of Jared, age 6
- First signs
- Treatments, procedures, and surgeries
- Complications: infections, accidents, bowel problems
- Catheterization: reactions and logistics
- How it affects our family life
- How it affects our child’s social life
- Working with schools around Cathing
- Mitrofanoff procedure: creating a catheterizable stoma
- Working with the medical team
- How we cope with stress
- How we help our child cope
- Systems of support: connecting with other families
- Considerations for long term healthcare
- Tricks of the trade
- Words of wisdom
Clinician Insights:
It’s important for families to know that this is not being instituted due to a failure of prior treatments or anything that the families did or didn’t do appropriately in the past. It is just another way of making their child healthy and well.
Stuart Bauer, MD, Senior Associate in Urology
- Our Urology experts
- Understanding our urology programs
- Clean Intermittent Catheterization (CIC)
- Conditions that may use CIC
- Getting started with CIC
- Integrating CIC into the lives of patients and families
- Addressing ongoing problems with CIC
- Challenges and rewards
A group of parents and health care providers has reviewed all of these contributions for appropriateness.The Self-Cathing Experience Journal was created by the Boston Children’s Hospital Departments of Urology and Psychiatry.
Editor’s note: Please keep in mind that every patient is different, and discussions of alternative treatments, complications, and timelines may not apply to you. Additionally, some families identify medications and products that work well for them. The Experience Journals do not endorse specific brands. Each individual is different, and we invite you to discuss products with your doctors and nurses to see if they are right for you.
